Health alert: Get to Know Your PCP!
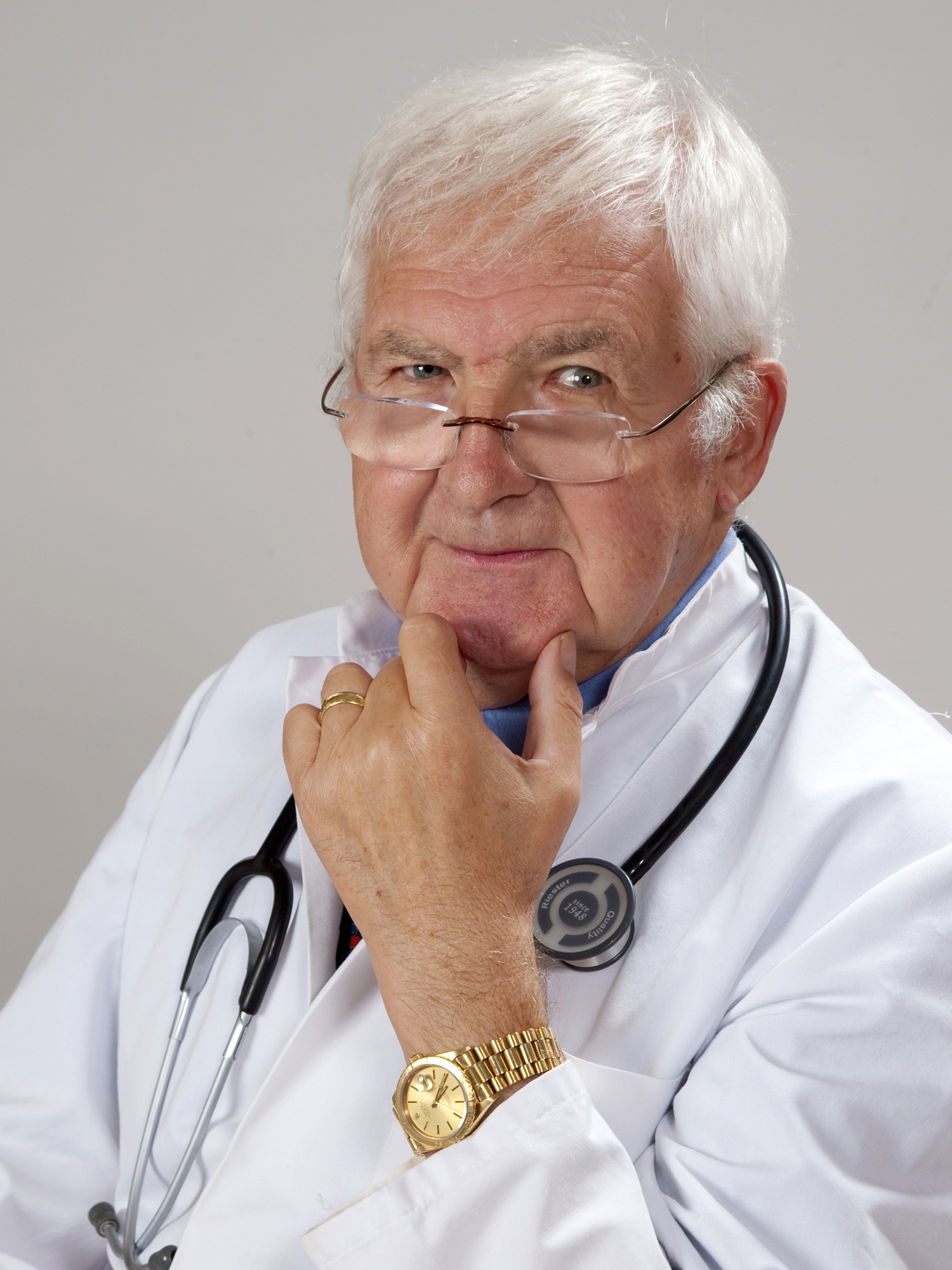
How well do you know your primary care physician (PCP)? Have you been with him/her for a long or a short time? How old do you think s/he is? How long in his/her practice?
These aren’t questions we’re inclined to spend time thinking about.
Maybe we, as third agers, should be more attentive to this relationship. Because there is an intensifying shift in the physician space that has been going on for a number of years that can affect our ability to get the care we may need as we get older.
If you’ve followed me for a while, you know I’m not a big fan of the healthcare system here in the U.S. (Note: my apologies to my non-U.S. followers. I’m going to be talking about what I understand to be largely a U.S.-centric issue).
If you are like most, your first point-of-contact when a health issue comes up is your primary care doc (PCP) who is most likely a primary care or family practice physician. They are generalists who treat adults (and children, in a family practice) specializing in the prevention, diagnosis, and management of disease and chronic conditions.
Like many things in life, we take them for granted, assuming they’ll be there when needed.
But that may be changing – and within our lifetime.
I’ve had a bit of a front-row seat to the machinations taking place in the healthcare space over the last 17 years as an executive healthcare recruiter. Over the last seven years, that involved recruiting specifically for small to large medical practices, some of which were internal medicine and family practice organizations.
When I moved my recruiting business to that healthcare segment, a major shift in the makeup of physician practices was well underway. Many independent medical practices, especially internal medicine and family practices, were struggling to survive because of the tremendous burden of regulations, insurance, and billing issues.
In particular, one of the major culprits in this shift was the advent of the electronic medical record system foisted on practices by the government. It has turned out to be one of the great disasters within our healthcare system history and is driving many physicians out of their practices.
Many internal medicine and family practices consolidated to try to achieve economies of scale. Or they scurried under the wings of hospitals to relieve the burden of running the office side of the business which stole from their ability to “be a doctor” and practice medicine.
Follow the money
For years, physicians-to-be have been selecting the more “prestigious” and higher-income specialties such as orthopedic, anesthesiology, dermatology and others and avoiding the family practice/internal medicine path. Much of this is being driven by the fact that primary care specialties are amongst the lowest-paying specialties.
It’s now becoming a national problem – one that could affect us in the coming years.
According to a 2019 study conducted by the Association of American Medical Colleges (AAMC) the United States will see a shortage of up to nearly 122,000 physicians over the next decade, including up to 55,000 primary care physicians.
Kaiser Health News recently reported that in 2019 the number of internal medicine positions offered was the highest on record – over 8,000. Only 41% were filled by graduating seniors pursuing their medical degrees from U.S. medical schools.
 So why am I sounding an alarm here?
So why am I sounding an alarm here?
Given this backdrop, we need to recognize that it’s going to be increasingly difficult to find a primary care physician that will accept us as a patient. Fewer are coming into the system and older docs are retiring out at an earlier age.
Burnout is a growing issue
Forty percent of males physicians and fifty percent of female physicians are burned out because of high patient loads, the hassles of running a practice, electronic medical record requirements, and government regulations – all while reimbursement rates under Medicare are declining.
This condition isn’t likely to get better, certainly not in our lifetimes.
So what is one to do? Here are three proactive things you may want to consider:
- Start by elevating your healthcare literacy. How much do you know about what all the parts and pieces of your body do, how they work, how they
 interact/interface/intertwine? Do you know the key biomarkers of your health and where yours are? How conscious are you of the insidious nature, positive and negative, of your current habits and the role they play in your long-term health? We exist inside of a 24×7 immune system of 35 trillion cells that are working hard to keep us healthy despite how we ignore and mistreat them. The knowledge to know how to provide them what they need to do their jobs has existed for a long time, but we give it up to complacency and convenience. That is, until a calamity hits.
interact/interface/intertwine? Do you know the key biomarkers of your health and where yours are? How conscious are you of the insidious nature, positive and negative, of your current habits and the role they play in your long-term health? We exist inside of a 24×7 immune system of 35 trillion cells that are working hard to keep us healthy despite how we ignore and mistreat them. The knowledge to know how to provide them what they need to do their jobs has existed for a long time, but we give it up to complacency and convenience. That is, until a calamity hits. - Take greater control of your own health. As an extension of number one, take full charge and responsibility for your health. I don’t believe that we should rely on our doctor to be the arbiter of our health. Rather, they should be our partners, with us at the helm. Our ability to do that does require an elevated healthcare literacy and a commitment to compliance. Too often in our culture, we play into the hands of a reactive healthcare system and turn to our docs only when something skids off the tracks. It’s like we’ve turned our healthcare into a reactive, $35 co-pay experience. Start now to let your PCP know that you are going to become, with his/her help, more knowledgeable about what it takes to be healthier and that you wish to partner with her/him on a plan of self-efficacy – taking charge of your health.
 P.S. You might get pushback from your doc. Here’s why: what you are asking of them doesn’t fit the corporate model that they have stepped into if they are part of a large health system or large consolidated practice. Expectations on the part of the system or practice are to see as many patients a day as possible. Follow the money. The more visits, the more insurance payouts. Someone like you with your questions and requests take time that your doc may want to take with you but be forced to avoid because of insurance restrictions and health system expectations. Plus a lot of what you will want to know and discuss doesn’t translate into the boxes in the electronic medical record that your doc has his nose in throughout your entire meeting. You are creating more “paperwork” for an already overburdened doc. It’s your health – don’t let all that get in the way.
P.S. You might get pushback from your doc. Here’s why: what you are asking of them doesn’t fit the corporate model that they have stepped into if they are part of a large health system or large consolidated practice. Expectations on the part of the system or practice are to see as many patients a day as possible. Follow the money. The more visits, the more insurance payouts. Someone like you with your questions and requests take time that your doc may want to take with you but be forced to avoid because of insurance restrictions and health system expectations. Plus a lot of what you will want to know and discuss doesn’t translate into the boxes in the electronic medical record that your doc has his nose in throughout your entire meeting. You are creating more “paperwork” for an already overburdened doc. It’s your health – don’t let all that get in the way.
- Know your PCP. How old is your primary care physician? How long is he/she planning to continue to practice? Have you asked her/him? You might want to just so you know in case you need to plan ahead for a replacement. We are seeing many PCPs retiring or selling their practice and going inactive at much earlier ages than in the past. Much of this is due to the declining incomes at the primary care level combined with, and often the result of, the challenges of managing a primary care practice and being a doctor at the same time. Don’t get caught having to scramble to find a PCP who will take you as a new patient. Obviously, because of reasons cited earlier, it will be tougher and you may be faced with settling for less than what you want in a doctor.
One possible solution to consider: a relationship with a concierge practice where, for an annual fee, you are guaranteed unlimited access to a doctor who really does want to practice medicine. The model is built on reducing patient enrollment from several thousand down to 5-600 and offering more personalized service.
One of the primary care docs I was with for a short while admitted to having 4,800 patient charts. The average appears to be around 2,500 for primary care physicians. Concierge-style practices can be relatively expensive, and there can be some insurance coverage issues, but I’m told it’s an environment where you can truly partner with your physician.
So, to recap.
We need that PCP but we needn’t relinquish our health to them. Be sure you are positioned with one that is going to be around for a while and engage him/her at a deeper level letting them know you are becoming more knowledgeable ( with her/his help), that you are taking charge, and really want his/her help on this journey.
I believe you will get a very positive response from the doctor. One, because they get that from very few; two, because you are asking them to do what they really want to do – be a doctor.
You will quickly discover, from the response, if this is someone you want to continue with –or whether it’s time to initiate a search for someone else.
This shortage is not likely to get the attention it needs from the government or, surprisingly, from the medical community itself. It’s lost, along with all the other critical issues that are going nowhere in Disneyland on the Potomac.
It’s on us. Don’t wait until it’s too late.
Let me know of your experience in this area – positive or negative. We welcome your feedback on this topic – scroll down and leave a comment below.




Hey Gary, great blog as always. Sue and I just recently changed to the same new PCP—-partly for the reasons you described. He’s young, bright, and eager to help us both stay healthy. And congratulations on #100. Well done!!
Great to hear from you, Danny. Thanks for the kudos. Hope you are able to stay with this doc for the long term – and may that long term be real long term. Best to Sue.
I am 64 and have lost all my long time doctors due to death or retirement. I have tried new doctors and have to say I dont feel a connection. Drugs are widely prescribed without homepathic alternatives, which I find on my own.
I worry about what will happen to the elderly with such a grey area in healthcare for the future.
It’s a valid worry Mary. Thanks for your comments. Working together, maybe we can elevate senior awareness of this impending physician shortage and the importance of taking charge of our health.
I real pleased to find this web site on bing, just what I was looking for : D as well saved to bookmarks.
This really answered my problem, thank you!